3D Bioprinting system /NIH In the last few years, the use of 3D printing has exploded in medicine. Engineers and medical professionals...
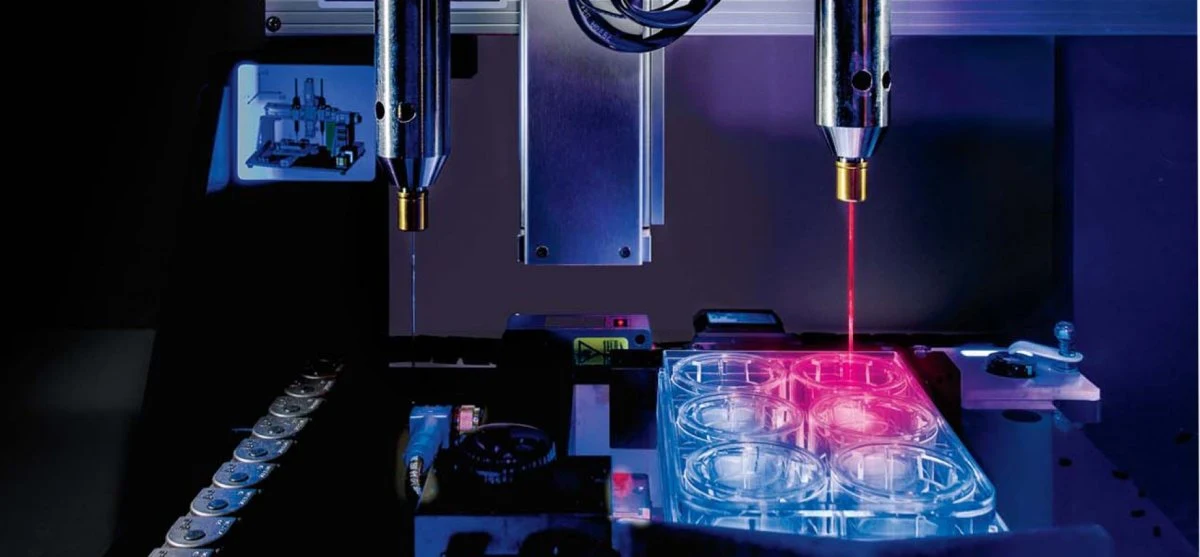 |
| 3D Bioprinting system /NIH |
Bioprinting and Why It Matters?
Bioprinting is a hot topic in medical science circles these days. After nearly two decades of existence, 3D printing has blossomed from a pigeonholed manufacturing tool into a thriving $2.7 billion dollar industry today. Using materials such as plastic, metal, or even chocolate, 3D printing has been responsible for the production of a wide variety of items, varying from different types of jewelry, car parts, food, to musical instruments.
Bioprinting creates three-dimensional structures of biological materials that replicate actual human cells necessary to produce organs that a normal body can recognize and naturalize. The ultimate goal of the new technology is to replicate fully functioning living cells, tissues and organs, which can then be transplanted into human beings.
Scientists have been tracking this developing industry and are now working to implement these same principles and process in the medical field. Before getting too excited one must realize that 3D printing using metal, plastic, and other materials is drastically less complex than reproducing living cells or tissues. This is not to say we won’t see bioprinting implemented in the medical industry in the near future, yet one must be much more cautious and patient in realizing that we are dealing with a living matter.
We have been mapping the adoption of 3D printing technologies in the field of health care, and particularly bioprinting, in a collaboration between the law schools of Bournemouth University in the United Kingdom and Saint Louis University in the United States. While the future looks promising from a technical and scientific perspective, it’s far from clear how bioprinting and its products will be regulated. Such uncertainty can be problematic for manufacturers and patients alike and could prevent bioprinting from living up to its promise.
From 3D printing to bioprinting
Bioprinting has its origins in 3D printing. Generally, 3D printing refers to all technologies that use a process of joining materials, usually layer upon layer, to make objects from data described in a digital 3D model. Though the technology initially had limited applications, it is now a widely recognized manufacturing system that is used across a broad range of industrial sectors. Companies are now 3D printing car parts, education tools like frog dissection kits, and even 3D-printed houses. Both the United States Air Force and British Airways are developing ways of 3D printing airplane parts.
 |
| Bioprinting for cells and biomaterials. |
State of the art in bioprinting
Bioprinting’s rapid emergence is built on recent advances in 3D printing techniques to engineer different types of products involving biological components, including human tissue and, more recently, vaccines. While bioprinting is not entirely a new field because it is derived from general 3D printing principles, it is a novel concept for legal and regulatory purposes. And that is where the field could get tripped up if regulators cannot decide how to approach it.
We expect that advancements in bioprinting will increase at a steady pace, even with current technological limitations, potentially improving the lives of many patients. In 2019 alone, several research teams reported a number of breakthroughs. Bioengineers at Rice and Washington Universities, for example, used hydrogels to successfully print the first series of complex vascular networks. Scientists at Tel Aviv University managed to produce the first 3D-printed heart. It included “cells, blood vessels, ventricles, and chambers” and used cells and biological materials from a human patient. In the United Kingdom, a team from Swansea University developed a bioprinting process to create an artificial bone matrix, using durable, regenerative biomaterial.
‘Cloneprinting’
Though the future looks promising from a technical and scientific perspective, current regulations around bioprinting pose some hurdles. From a conceptual point of view, it is hard to determine what bioprinting effectively is.
Consider the case of a 3D-printed heart, regulators have a number of questions to answer:
- Is it best described as an organ or a product?
- Or should regulators look at it more like a medical device?
- To begin with, they need to decide whether bioprinting should be regulated under new or existing frameworks and, if the latter, which ones. For instance, should they apply regulations for biologics, a class of complex pharmaceuticals that include treatments for cancer and rheumatoid arthritis, because biologic materials are involved, as is the case with 3D-printed vaccines?
- Or should there be a regulatory framework for medical devices better suited to the task of customizing 3D-printed products like splints for newborns suffering from life-threatening medical conditions?
Dolly the sheep’s example illustrates the court’s reluctance to traverse this path. Therefore, if, at some point in the future, bioprinters or indeed cloneprinters can be used to replicate not simply organs but also human beings using cloning technologies, a patent application of this nature could potentially fail, based on the current law. A study funded by the European Commission, led by Bournemouth University and due for completion in early 2020 aims to provide legal guidance on the various intellectual property and regulatory issues surrounding such issues, among others.
On the other hand, if European regulators classify the product of bioprinting as a medical device, there will be at least some degree of legal clarity, as a regulatory regime for medical devices has long been in place. In the United States, the FDA has issued guidance on 3D-printed medical devices, but not on the specifics of bioprinting. More important, such guidance is not binding and only represents the thinking of a particular agency at a point in time.
Cloudy regulatory outlook
Those are not the only uncertainties that are racking the field. Consider the recent progress surrounding 3D-printed organs, particularly the example of a 3D-printed heart. If a functioning 3D-printed heart becomes available, which body of law should apply beyond the realm of FDA regulations? In the United States, should the National Organ Transplant Act, which was written with human organs in mind, apply? Or do we need to amend the law, or even create a separate set of rules for 3D-printed organs?
We have no doubt that 3D printing in general, and bioprinting specifically, will advance rapidly in the coming years. Policymakers should be paying closer attention to the field to ensure that its progress does not outstrip their capacity to safely and effectively regulate it. If they succeed, it could usher in a new era in medicine that could improve the lives of countless patients.